SINGAPORE – Singapore has detected 14 cases of mpox since January 2024, but they all stemmed from the clade II virus that causes less severe infections.
Clade I causes more severe symptoms and a significantly higher fatality rate, and is circulating mainly in Democratic Republic of Congo.
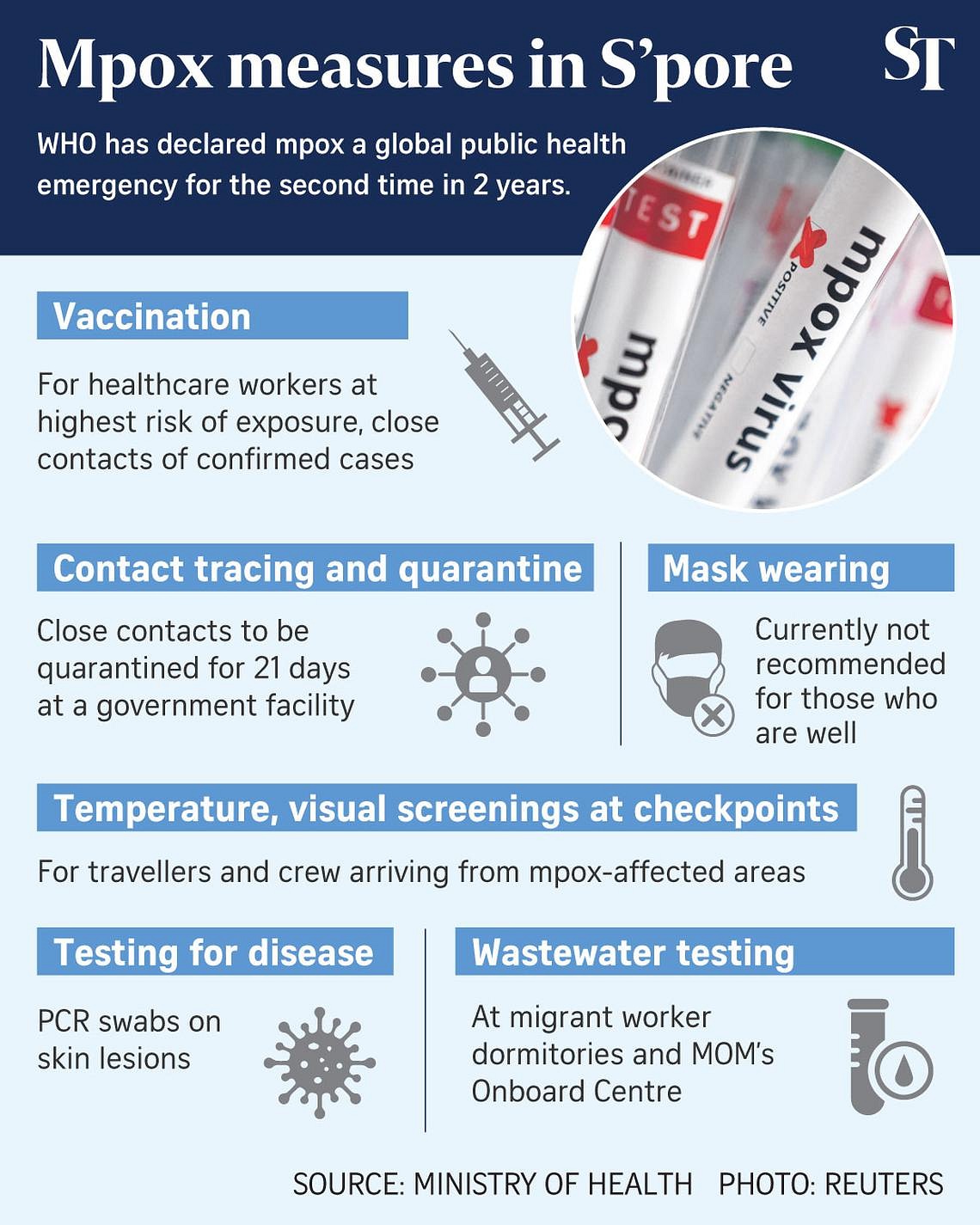
While there are currently no reported cases of clade I in the Republic, a slew of public health measures aimed at curbing the spread of mpox was announced on Sept 4 by Health Minister Ong Ye Kung.
These included contact tracing and quarantine, wastewater testing, as well as vaccinations for those at higher risk.
Despite mpox being unlikely to lead to the kind of widespread disruption that happened during Covid-19, Singapore is monitoring the global situation closely and is ready to respond decisively should it change, he said.
Q: Why is the vaccine against mpox not being given to everyone?
A: Jynneos is a live, non-replicating vaccine approved for use in Singapore against smallpox and mpox.
It is being given free to healthcare workers at highest risk of exposure to the virus, such as those at the National Centre for Infectious Diseases (NCID) who would be in close contact with mpox patients, said Professor Kenneth Mak, director-general of health at the Ministry of Health (MOH).
Another group that will be given the jabs free are the close contacts of confirmed cases. This is to ensure that the people who need them most will be given protection.
Most Singaporeans born in or before 1980 were already vaccinated against smallpox in childhood. As smallpox and mpox come from the same family of viruses, the vaccine provides some cross-protection.
Based on this current vaccination approach, the existing supply in Singapore is projected to be sufficient, Prof Mak said. “To better strengthen our preparedness and resilience, MOH is looking at procuring more doses when available and (will) adjust our vaccination strategy as needed.”
Q: Can Singapore use lessons from the Covid-19 pandemic to curb a possible mpox outbreak here?
A: Health Minister Ong Ye Kung on Sept 4 cautioned that Singapore must “never fall into the trap of fighting the last war” and assume strategies used to fight Covid-19 can be used to handle mpox clade I, as every virus has its own characteristics.
However, existing measures against infectious diseases are relevant to prevent the spread of mpox clade I, he said.
These include maintaining good hygiene practices, conducting visual screening for symptoms, and outbreak management measures like isolation, contact tracing, decontamination of premises and temporary closure.
Temperature and visual screening are in place at the airports and sea checkpoints for inbound travellers and crew arriving from places where they may have been exposed to mpox clade I outbreaks.
Suspected cases of mpox will be transferred to hospitals and isolated, pending test results. Those who test positive for clade I will continue to be isolated in healthcare facilities until they are no longer infectious.
Unlike for Covid-19, contact tracing for mpox will be done physically and not using TraceTogether.
In addition, wastewater testing at migrant worker dormitories and the Onboard Centre will be carried out to prevent any spread within their living quarters.
Q: How would a doctor tell if the rash I have is a symptom of mpox?
A: Dr Shawn Vasoo, clinical director of NCID, said it can be challenging sometimes differentiating mpox from other forms of rash if there are few lesions.
“As part of healthcare worker education, NCID has held webinars (in September) with primary care physicians to share the clinical evaluation and management of mpox patients, and further outreach is being planned. A joint NCID-MOH guidance on mpox with visual aids has been issued to healthcare professionals for mpox in 2022 and with an update in 2023. A refreshed guidance for 2024 is also under way,” he said.
Dr Vasoo said mpox rash typically develops in five stages, from flat, red spots to hard, raised bumps, then blisters filled with clear fluid to blisters filled with pus, before crusting over and becoming scabs that gradually fall off.
The rash, he said, is different from chickenpox, which happens in multiple stages of development, and measles, which is usually flat or slightly raised, red spots. “Persons with mpox are also more likely to have swollen lymph nodes, which is typically not as prominent with chickenpox or measles,” he added.
Professor Paul Tambyah, president of the International Society for Infectious Diseases, said: “GPs (general practitioners) have all been briefed and should be able to identify suspect cases and refer them as needed. The rashes can also be in the throat, groin and genital areas, so those also need to be looked at as well.”